Most people don’t think something is seriously wrong. It usually starts with small symptoms. A strange heaviness after eating. No food craving. Your jeans become loose, but you are not on a diet. You tell yourself it’s nothing or think maybe you are in stress, maybe an age factor or maybe something you ate wrong! That’s how pancreatic cancer often begins. By the time the word cancer enters the conversation, many people are already exhausted — from symptoms, from uncertainty, and not being taken seriously early enough.
This article isn’t to scare you. It’s here to explain things the way doctors often don’t have time to.
Slowly and honestly. Just one to one.
So… What actually Pancreatic Cancer is?
Pancreas, It’s one type of main part in the body. An organ that needs proper care. If anything goes wrong, it doesn’t announce problems the way the heart or lungs do. It just works. Until it doesn’t.
Works behind the stomach, helps to digest food and keeps blood sugar stable. When cells are going out of control, the cancer cell develops inside. Due to the pancreas being very deep in the body, tumors can grow quietly. No visible swelling. No early warning pain. Just subtle changes that are easy to brush off. That’s not negligence. It’s human nature.
Pancreatic Cancers and Types - Not Same always!
It’s true! And this part matters more than people realise. Most cases are pancreatic adenocarcinoma. This type starts in the ducts that carry digestive enzymes. It tends to behave aggressively and often gets detected late.
Then there are neuroendocrine tumors. These are rarer. Sometimes slower. Sometimes easier to manage. Some people live with them for years.
Doctors approach these two very differently. That’s why a clear diagnosis is important.
Symptoms of Pancreatic Cancers
Here’s the uncomfortable truth. Early pancreatic cancer symptoms don’t feel dramatic. They feel familiar.
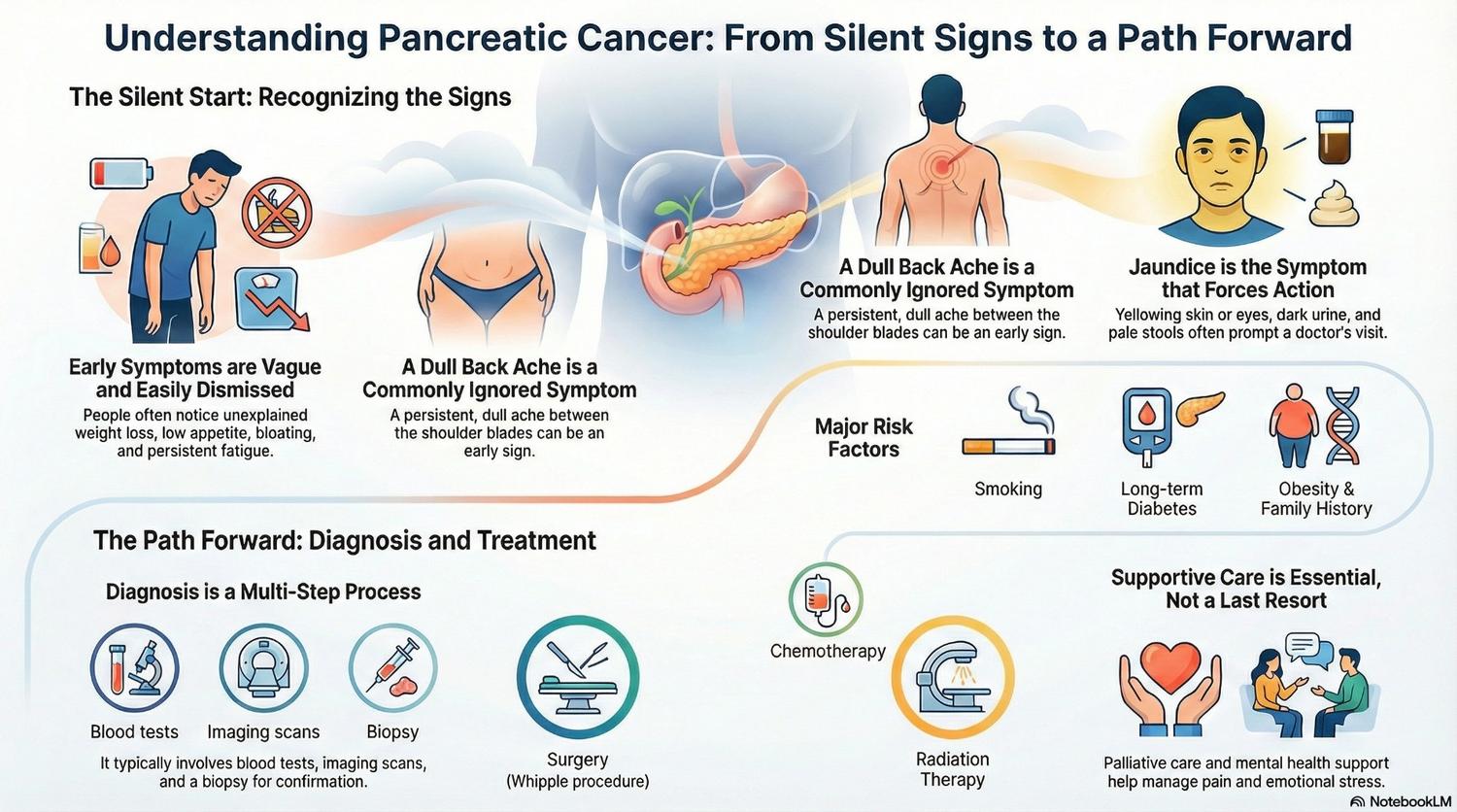
People notice:
• Appetite slowly dropping
• Weight slipping off without effort
• Bloating that doesn’t quite settle
• Fatigue that coffee doesn’t fix
Nothing feels urgent. So people wait.
The Back Pain is ignored by many people!
Many patients later remember a dull ache in their back. Somewhere between the shoulders. Not sharp and not constant. Just… there. It comes and goes. So it gets ignored.
Jaundice Changes Everything
Yellow eyes or skin tend to stop the waiting. Dark urine and pale stools. It’s often the first symptom that forces medical attention. But by then, the disease may already be advanced.
When Things Start Feeling Serious
As the cancer grows, the body struggles to compensate.
• Pain becomes harder to ignore.
• Eating feels like a chore.
• Weight drops faster.
• Some people may diagnosed with diabetes
At this stage, doctors prescribed scans, stages, and dedicated treatment plans.
Main causes that lead to Pancreatic Cancer
It’s not as simple as you think!. Anyone who gives one is oversimplifying. But doctors know certain things raise risk:
• Smoking
• Long-term diabetes
• Chronic inflammation of the pancreas
• Obesity
• Family history or genetic mutations
• Age
None of these guarantee cancer. They just mean symptoms deserve attention sooner.
How Doctors Actually Diagnose It
Blood tests raise suspicion. Scans show something unclear. Another scan follows. Then maybe an endoscopic test is required. Sometimes a biopsy helps! Sometimes symptoms worsen and this diagnosis process feels slow.
That’s why experienced centers matter. And why second opinions aren’t insults — they’re safeguards.
What Do “Stages” Really Mean?
Staging sounds technical, but it answers one basic question:
How far has this gone?
• Early stages mean the cancer is still contained
• Later stages mean it has reached blood vessels or distant organs
Doctors also talk about whether surgery is possible. That decision shapes everything that follows.
Patients Experience During Treatment
One treatment is not the same for all and it’s rarely straightforward.
• Surgery – Surgery offers the best chance when possible. The Whipple procedure is complex. Recovery is slow. But in some cases, it may change everything.
• Chemotherapy – Chemotherapy is a good option as per the patient situation. Side effects vary widely. Some people tolerate it better than expected. Supportive care matters here more than people admit.
• Radiation and Newer Treatments – Radiation sometimes helps control growth. Newer targeted treatments work for certain genetic profiles. Clinical trials open doors for some patients.
• Palliative Care (And Why It’s Misunderstood) – Palliative care isn’t giving up. It’s about comfort. Pain control. Better digestion and better sleep. It can help at any stage.
Survival, Statistics, and Reality
Survival rates are numbers. People are not, but the stage matters. Treatment response matters. Overall health matters and access to good care always matters. Statistics help doctors plan and
They don’t predict individual lives.
Living With the Diagnosis
Life doesn’t stop after diagnosis. It just changes. Eating may require enzymes. Energy comes and goes. Fear sits quietly in the background but ignores the negative sites. This is the most important. Mental health support isn’t optional here. It’s part of treatment. And caregivers — often spouses or children — carry more weight than anyone sees. They need care too.
Conclusion:
Pancreatic cancer is hard. Not just medically. Emotionally. Mentally. Practically. But clarity helps people breathe again. Understanding brings some control back. And no one should feel lost while navigating this.





